Family Medicine in Canada: Scope of Practice and Clinical Autonomy Explained
Internationally trained General Practitioners (GPs) considering practice opportunities in Canada, frequently have two dominant concerns at the outset of their search for positions: the scope of clinical practice and level of clinical autonomy afforded by the job.
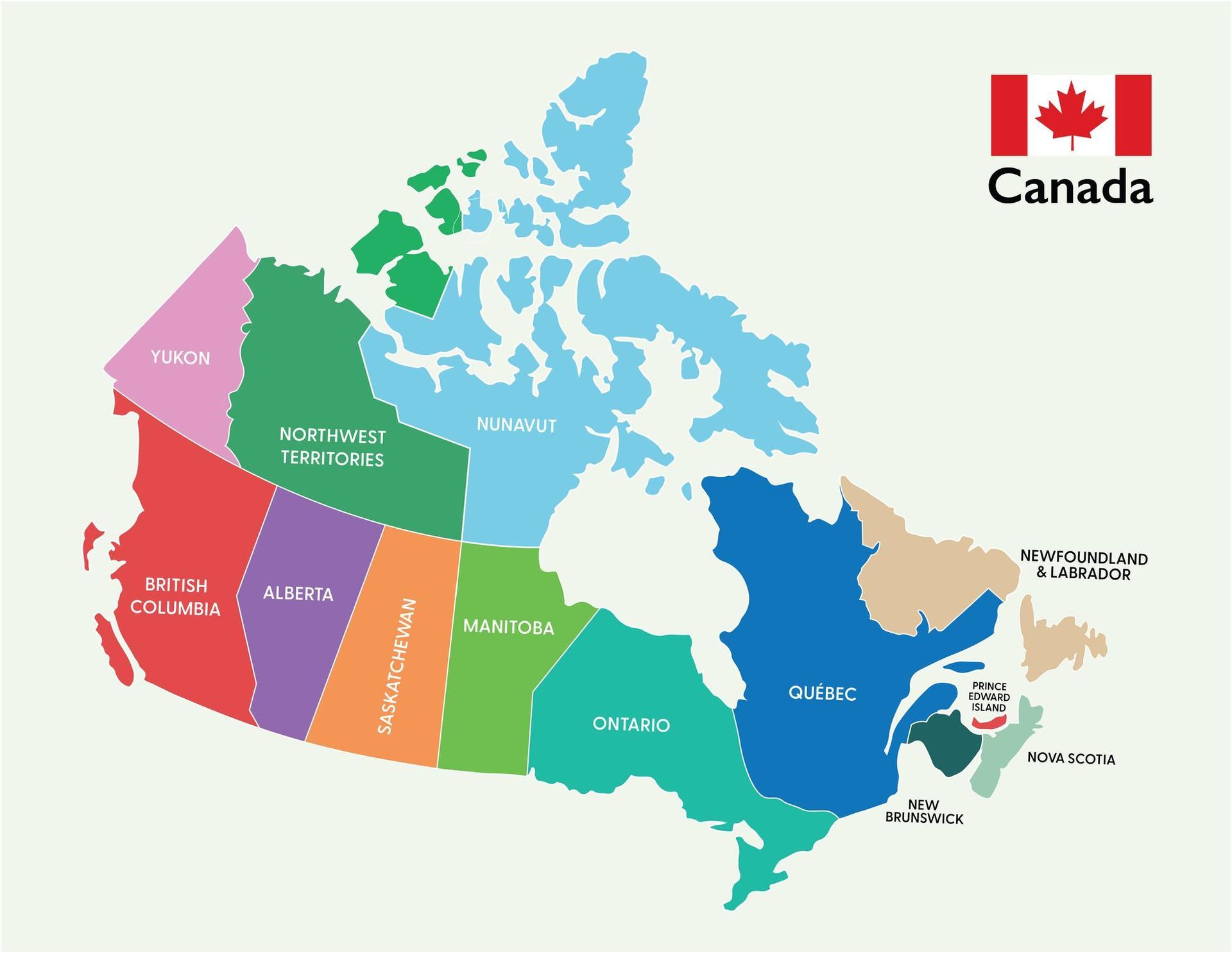
Fortunately the responses are usually straightforward. Canada offers some of the broadest and most autonomous scopes of practice for Family Physicians globally. However, that scope varies by province, medical practice, community size, and individual physician preference.
This article provides a detailed overview of what GPs can expect in terms of clinical responsibility, procedural work, hospital involvement and professional independence.
1. The Role of the Family Physician in Canada
Family Physicians form the cornerstone of Canada’s publicly funded healthcare system acting as the gatekeeping layer between primary and secondary care. Patients needing specialist opinion require referral from a GP to access publicly funded specialist care.
Unlike some healthcare systems where primary care is narrowly defined, Canadian family medicine is designed to be comprehensive and continuous. GPs have considerable clinical autonomy and the ability to determine their preferred schedules and scope of practice with opportunities to develop enhanced procedural and secondary skills rarely available in other countries. This is particularly relevant to physicians seeking practice opportunities in the more remote areas of this vast country.
In most provinces, family physicians function as comprehensive primary care providers, assessing and treating patients of all ages from infancy to old age. This includes the management of chronic disease, preventative medicine and in some areas, basic hospital care, minor surgery, anaesthesia, obstetrics and emergency medicine.
2. The Core Scope of Family Medicine Practice
Family physicians enjoy work scheduling autonomy. Most physicians maintain patient panels between 1,200 and 1,800 patients depending on practice model. Patient appointment lengths typically range from 10–20 minutes.
The basic scope of practice includes:
- Acute illness management
- Chronic disease management (diabetes, hypertension, COPD, heart failure)
- Mental health (depression, anxiety, ADHD, addiction medicine)
- Women’s health and contraception
- Antenatal and postnatal care (varies by region)
- Paediatrics
- Geriatrics
- Palliative care
- Preventive screening and immunisation
3. Procedural Scope
One of the defining features of Canadian family medicine, particularly outside major metropolitan centres, is the opportunity to develop and maintain procedural skills. Expanded procedural scope directly influences earning potential under Fee-for-Service models with procedure fees generally higher than those for consultations.
Common office-based procedures include:
- Skin excisions and biopsies
- Joint injections
- IUD insertions
- Vasectomies (in some practices)
- Cryotherapy
- Minor surgical procedures
In rural settings, additional skills may include:
- Emergency medicine coverage
- Obstetrics (including deliveries)
- Inpatient care
- Anaesthetic services (with additional certification)
- First assist in surgery
4. Urban vs Rural Scope
Urban practices tend to prioritise patient consultations, chronic disease management and other standard primary care services over enhanced skills and procedural competency, which are personal options rather than essential skills. Specialist referral is close at hand hence there is less need to manage complex cases, perform urgent procedures or attend to hospitalised patients. Patient panels can be large and demanding and appointment schedules intensive.
Urban medical clinics are often the best starting point for physicians new to the Canadian primary care services. Collegial support is crucial to successful integration into the system.
Rural medicine in Canada often resembles a hybrid of general practice and community hospitalist medicine where GPs frequently manage hospitalised patients, work shifts in emergency departments and even practice obstetrics and anaesthesia, performing basic surgical procedures. A greater level of clinical autonomy is usual but this must be accompanied by both competence and confidence as collegial support is limited and secondary care many miles away. Additional courses may be undertaken to acquire the supplementary skills required for this type of work.
5. Employment Structure and Autonomy
Most Canadian Family Physicians join clinics or medical practices and operate as independent contractors. They bill provincial health insurance plans directly and pay over heads to the clinics to cover property and administrative costs. This arrangement is called a fee split, with 20-30% of the total fees paid to the clinic.
Under this system, physicians enjoy substantial professional autonomy with the ability to select patient panel size, determine clinic schedules and procedural scope. Some choose to incorporate for tax efficiency.
6. Financial Compensation Models
The fee for service model remains the most common financial compensation model but capacitation and blended models are gaining popularity. Both models possess advantages and disadvantages.
Fee-for-Service (FFS)
Gross fee income is tied directly to the clinical volume of work and the total fee value of consultations and procedures performed. This rewards effort and acts as a motivational incentive but can lead to income fluctuation over the course of time.
Capitation or Blended Models
In these models, income is partially based upon the number of registered patients (capitation) with fees for each item of service or fixed fees for sessional work. These modes are less dependent upon the quantity of services provided and reduce the pressure on the physician to maintain high daily patient volumes. The disadvantage is the lowering of maximal earnings.
Some provinces, such as British Columbia, have introduced reformed models which financially compensate for time spent, patient complexity and administrative work.
7. Team-Based Care
Canadian primary care increasingly operates within multidisciplinary teams. Family Physicians retain overall clinical responsibility but collaborate within team-based care models.
Depending on province and funding structure, clinics may include:
- Nurse practitioners
- Registered nurses
- Pharmacists
- Social workers
- Dietitians
- Mental health counsellors
8. Hospital Privileges and Inpatient Care
In urban settings, inpatient care is often managed by hospitalists. Family physicians can chose to maintain hospital privileges or relinquish them to focus on their clinic work. In some provinces and rural regions, family physicians may:
- admit and manage inpatients
- provide maternity care
- cover emergency departments
9. Professional Regulation and Standards
Family Physicians must hold licensure through their provincial College of Physicians and Surgeons and hold board certification with the College of Family Physicians of Canada. The College also overseas Continuing Professional Development (CPD) requirements which are mandatory for all family physicians.
10. Comparison With the UK and Australia
| Feature | Canada | UK | Australia |
|---|---|---|---|
| Employment | Independent contractor | Partner / Salaried | Independent contractor |
| Scope breadth | Broad (esp. rural) | Narrowing | Broad (esp. rural) |
| Hospital privileges | Possible | Rare | Possible |
| Income ceiling | High | Moderate | High |
| Administrative Burden | Moderate | High | Moderate |
Conclusion
For experienced General Practitioners seeking professional independence, high incomes and diverse clinical exposure, Canada offers one of the most attractive primary care environments internationally.
19 February 2026
Share this post on Social Media