How Primary Care Works in Canada: A Guide for International General Practitioners
Canada offers one of the most stable and professionally rewarding environments for General Practitioners (Family Physicians) globally. However, the structure of primary care differs in important ways from the UK, Ireland, Australia and other Commonwealth systems.
This guide provides a comprehensive overview of how primary care operates in Canada, including funding, remuneration, practice models, referral systems, and rural medicine, specifically for internationally trained GPs exploring employment opportunities in Canada.
1. The Foundation: Publicly Funded, Provincially Delivered Healthcare
Canada operates a publicly funded healthcare system governed by the Canada Health Act, whereby eligible residents of Canada must have reasonable access to essential health services defined as insured health services and extended healthcare services. Insured health services include medically necessary hospital, physician and certain surgical-dental services. Extended health care services include certain long-term care services including nursing home care and adult residential care.
The act sets out the criteria and conditions for the coverage of both types of services which must be provided on the same terms and without patient charges across the country. However, each province and territory administers its own health services, and must meet the conditions set out in the Act to receive their full federal cash contribution under the Canada Health Transfer.
This decentralised model differs from the publicly funded National Health Service (NHS) in the United Kingdom with implications for both financial compensation and professional regulation of general practitioners.
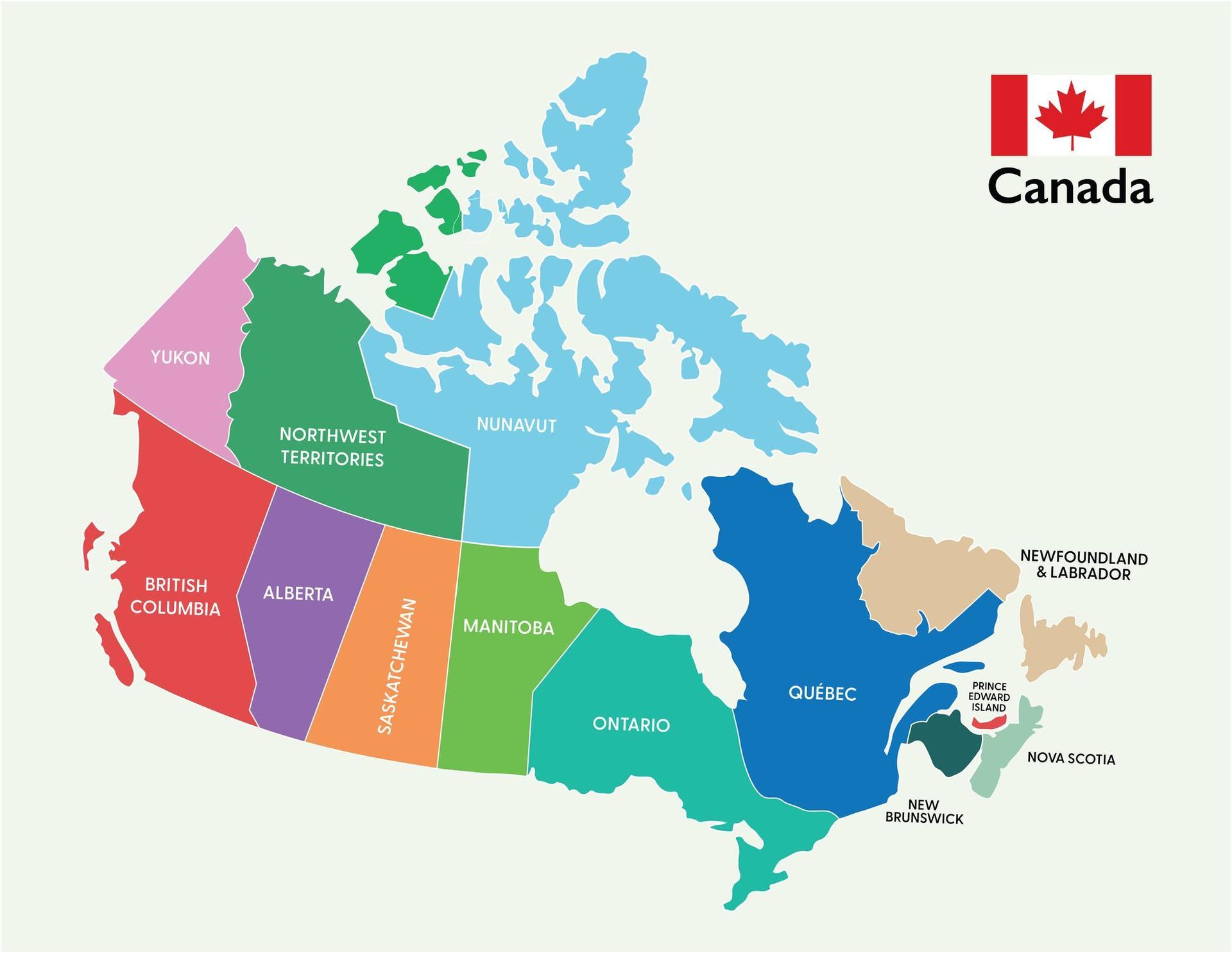
Family Physician licensing is provincial or territorial and not national, therefore separate licenses are required to practice in each province. Similarly, physician payment models are determined provincially with wide disparities in remuneration across the country.
2. The Role of the Family Physician in Canada
Family Physicians are the cornerstone of the Canadian healthcare system. Working in clinics as independent contactors rather than salaried employers, their scope of practice is extensive and often encompasses a broader procedural scope than their counterparts in the UK.
The scope of practice includes:
- Comprehensive primary medical care from infancy to old age
- Specialist referrals
- Chronic disease management
- Preventive medicine and screening
- Women’s health and antenatal care
- Minor surgical procedures
- Psychiatry
- Palliative care
- Hospital privileges (in some regions)
- Emergency or urgent care (especially rural settings)
- Obstetrics (in some rural practices)
3. Practice Structure: Independent Contractor Model
In contrast to NHS GP partnerships, Canadian clinics are typically corporate entities or physician-owned group practices rather than equity partnerships. Most Canadian family physicians operate as independent contractors and bill the provincial health insurance plan directly on a fee for service basis, paying a percentage overhead to the clinic (commonly 20–30%) to cover administrative expenses. Salaried positions exist but are quite rare.
Income is therefore activity dependent and can be enhanced by the performance of procedures or undertaking additional clinical sessions. Income potential is generally higher than in the UK with greater control over scheduling and patient volumes.
4. How GPs Are Paid: Fee-for-Service vs Alternative Payment Models
Fee-for-Service (FFS)
This is the traditional model and still the most common form of family physician financial compensation. Physicians bill per consultation or procedure according to a provincial fee schedule and are reimbursed accordingly. Transparent and straightforward with a direct correlation between workload and income, this model offers high earning potential but income variability.
Alternative Payment Plans (APPs)
Many provinces now offer alternative financial compensation models to the standard free for service model. Occasionally these are salaried posts but more commonly a blend of different models including session based payments or capitation payments (payment per registered patient), often mixed with a fee for service component.
For example:
- Ontario offers Family Health Organizations (FHO) models.
- British Columbia has Longitudinal Family Physician (LFP) payment reforms.
- Alberta provides both FFS and Primary Care Network models.
The choice of financial compensation model significantly impacts income, work-life balance and administrative burden.
5. Referral Pathways and Specialist Access
As in the UK, family physicians act as gatekeepers to secondary care and refer patients to selected specialists when appropriate. Referrals are required for publicly funded specialist access, although not necessarily for private specialist consultations. Wait times vary considerably by province and specialty and lengthy waits are common in fields and regions where specialists are in short supply.
Family physicians may directly order diagnostic radiological and laboratory investigations, particularly ultrasound, CT, MRI and standard blood tests. In rural areas, GPs may assume extended responsibilities due to limited specialist availability and some manage hospital in patients and perform obstetric procedures.
6. Rural and Remote Medicine in Canada
Rural Canada faces significant physician shortages and family physicians are often attracted to work in these areas by financial inducements and the opportunities to enhance their skills and assume greater levels of responsibility and specialist practice. Financial benefits include relocation packages, sign up bonuses, retention bonuses, housing support, higher billing incentives and provincial recruitment grants. The Atlantic provinces offer an accelerated route to permanent residency for physicians willing to sign up for 2 years.
In these settings, Family Physicians may provide emergency medicine coverage, manage telemedicine consultations and services, practice obstetrics, perform minor surgery and provide anaesthetic services (with additional training).
7. Workload and Appointment Structure
Appointment lengths are generally shorter than UK standard GP appointments with a typical structure of 10-15 minute appointments, 25–40 patients per day (depending on practice style) and flexible scheduling determined by the physician. Evening or weekend clinics are common in some urban centres.
There is no national mandate on patient panel size. Many GPs maintain 1,200–1,800 patients, though this varies widely.
8. Medical Liability Protection
Canadian physicians obtain protection through the Canadian Medical Protective Association (CMPA).
CMPA provides medico-legal defence and advisory services rather than traditional indemnity insurance.
Fees vary by province and scope of practice but are often partially reimbursed by provincial governments.
9. Income Expectations
Income varies significantly by province and workload.
Approximate gross annual billings:
- Urban FFS GP: CAD $300,000–$450,000+
- Rural GP with expanded scope: CAD $400,000–$600,000+
- Alternative payment models: CAD $250,000–$400,000
After overheads (20–30%), net income remains highly competitive internationally.
Incorporation can provide additional tax efficiency.
10. Comparison with the UK NHS Model
Canadian practice is often perceived as more entrepreneurial, with greater financial upside but increased personal responsibility.
| Feature | Canada | UK |
|---|---|---|
| Employment status | Independent Contractor | Partner or Salaried |
| Payment | Fee-for-service or capitation | Global sum + QOF |
| Gatekeeping | Yes | Yes |
| Private practice | Limited | More Established |
| Earnings Ceiling | Higher Potential | Capped by Contract |
| Administrative Burden | Moderate - High | High |
11. Provincial Variability
Each province has unique characteristics and these should be understood before deciding upon preferred practice locations. The selection of province determines the licensing pathways and requirements and practice opportunities available.
- Ontario – Large population base, blended capitation models
- British Columbia – recent primary care payment reforms
- Alberta – strong rural incentives
- Nova Scotia – active recruitment of international physicians
- Saskatchewan & Manitoba – PRA pathways and underserved opportunities
- Newfoundland - a mixture of salaried and fee for service opportunities
12. Key Considerations Before Applying
Primary care in Canada offers exceptional professional autonomy, competitive incomes, and diverse clinical scope, but success depends on careful province-specific planning. International GP candidates should evaluate the following issues and then select a province as the focus of applications:
- Eligibility for a professional licence in each province
- Provincial licensing timelines and pathways - Practice Ready Assessment (PRA) or board eligibility
- Immigration route (work permit vs permanent residency)
- Payment model preference
- Rural vs urban lifestyle
- Long-term settlement goals
Conclusion
Canada’s primary care system is decentralised, physician-led, and financially rewarding. For internationally trained General Practitioners, it represents a structured but achievable pathway to relocation and long-term career development.
Understanding the independent contractor model, billing systems, and provincial differences is essential before embarking on licensure and immigration. For GPs seeking clarity on licensing, visa options, and live-market vacancies across Canada, a structured recruitment pathway significantly reduces risk and delays.
16 February 2026
Share this post on Social Media