Canada's Healthcare Crisis Caused by Lack of Staff and Funding
Canada is one of the world's richest countries with a publicly funded universal healthcare system, often touted as one of the best in the world. However critical staff shortages are creating a crisis with some emergency departments unable to stay open.
In mid August 2022, a general hospital located just two hours' drive west of Toronto, Ottawa (Canada's most populous province) was forced to close the doors of its emergency department. A note posted on the entry of the department said the emergency department was closed for the day. It would reopen the following morning at 08:00, but close again for the evening. Patients who needed urgent care were asked to go to nearby hospitals - a 15- to 35-minute drive away.
This was the ninth time since April 2022 that the Huron Public Healthcare Alliance, a network of four hospitals serving around 150,000 people in western Ontario, had to temporarily close or cut back hours at one of its emergency departments. And the reason? There is a shortage of nurses to staff the emergency department.
This is a common situation, replicated throughout Canada, particularly at smaller hospitals where reduced services have become commonplace. In the Atlantic maritime province of Nova Scotia, one hospital's emergency department has been closed since June 2021 due to staffing shortages.
Canada's Healthcare System.
Canada is one of the richest countries in the world with a strong economy, abundant natural resources and a high standard of infrastructure. Its universal publicly funded healthcare system has been touted by progressive politicians in the US, the country's southern neighbour, as a desirable alternative to the American system where millions of people remain uninsured.
Canada has a decentralized, universal, publicly funded health system called Canadian Medicare. Health care is funded and administered primarily by the country’s 13 provinces and territories. Each has its own insurance plan, and each receives cash assistance from the federal government on a per-capita basis. Benefits and delivery approaches vary. All citizens and permanent residents, however, receive medically necessary hospital and physician services free at the point of use. Some citizens and permanent residents may have to pay for excluded services, including outpatient prescription drugs and dental care. Provinces and territories provide some coverage for targeted groups. In addition, about two-thirds of Canadians have private insurance.
The modern version of Canada's universal healthcare system created under the Canada Health Act, has existed since 1984, although its roots were laid decades earlier in the province of Saskatchewan. Britain's National Health Service, established in 1948, served as the inspiration.
A 2021 report by the Commonwealth Fund "Mirror, Mirror 2021: Reflecting Poorly Health Care in the U.S. Compared to Other High-Income Countries" ranked Canada's healthcare system just one level higher than the USA. The study made an analysis of 71 performance measures across five domains drawn from Commonwealth Fund international surveys conducted in each country and administrative data from the Organisation for Economic Co-operation and Development and the World Health Organization. These were:
- access to care
- care process
- administrative efficiency
- equity
- health care outcomes
The top-performing countries overall are Norway, the Netherlands, and Australia. Canada's performance lagged in the areas of access to medical care, equitable care and outcomes.
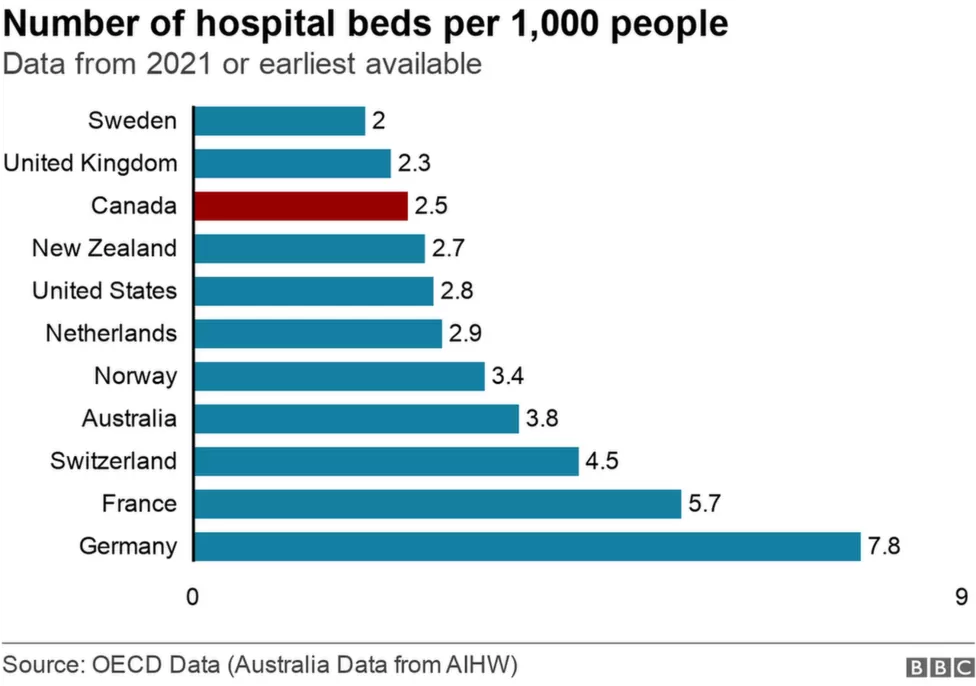
The OECD Data from 2021 compares hospital beds per 1,000 population between countries. Canada has just 2.5 beds per 1,000 people, placing it near the bottom of OECD countries, just ahead of the UK and Sweden.
The Current Crisis
Data over the last five years has shown that people are waiting longer in the Emergency department before they are either seen by a doctor or admitted to hospital. Nearly five million (just under 10% of the population) Canadians do not have a family doctor, often making an emergency room their primary place to get help if they need it.
In recent months, Canada's system has been described by workers and hospital executives as being in a state of "crisis". This includes struggling emergency rooms, long waits in the emergency department for attention and eventual hospital admission.
Emergency physicians in Toronto have noted stretchers lining the hallways, occupied by patients suffering from multiple ailments including fractured bones. On some days, those patients may wait anywhere from two to four days to be admitted to hospital wards for further treatment. Other patients are examined in the waiting room because the lack of staff has forced parts of the emergency department to close, with a consequent loss of privacy.
In the prairie province of Saskatchewan, some paramedics have spent the entirety of their 12-hour shift waiting with a patient on a stretcher as no one was around to admit the patient for treatment, leaving the paramedics unavailable to respond to other calls. Similar situations have been reported across the country from British Columbia to New Brunswick.
The Causes of the Crisis
The challenges brought on by Covid-19 bear part of the blame. Many nurses in Canada, fatigued from the pandemic, and the extra workload, have said they plan to leave the profession due to burnout and limited support. Many have retired or reduced working hours. Similar sentiments have been expressed by nurses in the US and in the UK, where a strike vote over wages is looming.
However many experts say that decades of poor policies, including the closure of hospitals and past austerity budgets, coupled with Canada's vast and complex geography, have exacerbated the pandemic pressure and lead to the current crisis.
This has ignited a national debate on how to recruit and retain staff, primarily nurses, and how to save a cherished public health system that is facing mounting pressure as it tries to care for an ageing population. Over the years, as Canada's population grew in size and age, its healthcare capacity struggled to keep up. Rural hospitals, where it can be a challenge to recruit staff, have been most affected.
The situation is exacerbated by a vacuum of nursing talent which existed before the pandemic. There were 34,315 vacant nursing jobs in Canada at the end of 2021, a 133% increase from 2019. It is estimated that Canada will be short of 117,600 nurses by 2030. A third of the current workforce is close to retirement, and in a 2021 national survey, nearly 60% of early-career nurses say they are considering leaving their current job.
The shortcomings of the system are most visible in the Emergency Department because it is the first port of call for most patients arriving at hospital with acute conditions. Closing the Emergency Department is never an easy decision, but a poorly-staffed department can be dangerous. However this has knock on effects as a closure at one emergency department means a bigger backlog at another one nearby. Some patients end up leaving without being seen by a doctor or a nurse, aggravated by lengthier-than-usual wait times.
The Autumn 2022 has brought an earlier than usual start to the annual respiratory virus wave of infections and has impacted children badly with an early surge in paediatric respiratory syncytial virus placing additional burdens on paediatric emergency services, in patient beds and intensive care facilities. Some paediatric emergency departments st up to manage 60 visits per day are already seeing 120 children daily.
Solutions to the Crisis
Prime Minister Justin Trudeau has said that Canada's public health care system "is one of the greatest things" about the country, and that his government is committed to working with provinces to "ensure Canadians get good, quality" care.
However the challenge of healthcare policy is that decision makers tend to focus on short-term solutions rather than larger overhauls that can increase access to everyone in the long term.
Politicians in all thirteen Canadian provinces have demanded increased federal funding of healthcare. Provinces are responsible for the healthcare system in their respective jurisdictions, though they rely on funding from the federal government.
Other solutions proposed include increasing wages for existing nurses, allowing internationally-educated nurses to practice in Canada, and increasing the capacity of nursing schools across the country, especially in rural areas.
Others have called for funding to be increased for care based in the community, so that people can access help before they end up in the Emergency Department and a drive for the recruitment of family physicians.
How to Apply for Medical Jobs in the Canadian Healthcare Sector
Candidates interested in working in medicine or healthcare in Canada, are invited to:
- register a CV
- contact us to discuss opportunities
- search for jobs
- read about details of professional registration with the medical regulatory authorities discussed in our article and more topics of interest can be found in our Resouces and Canada sections.
1 November 2022
Share this post on Social Media